Abstract
Introduction: Sickle cell disease (SCD) is one of the most prevalent monogenic hematological disorders leading to progressive multi-organ damage and reduced life expectancy despite a significant improvement of conventional and supportive care. Allogeneic hematopoietic stem cell transplantation (HSCT) with a matched sibling donor (MSD) represents currently the only curative treatment option, limited by a donor availability <20%. In a pilot study, we compared α/β/CD19 and CD3/CD19, respectively T-cell depleted haploidentical HSCT (T-haplo-HSCT) with MSD HSCT in patients (pts) with advanced stage SCD, using almost identical HSCT regimens for both donor groups.
Neurotoxicity (NT) contributes significantly to HSCT-associated morbidity and mortality. Calcineurin inhibitor (CNI) related NT after HSCT is mostly caused by cyclosporine A (CsA) and tacrolimus (FK506) with an overall frequency between 4.2% - 28.8%, and severe NT in 4% - 11%, such as posterior reversible encephalopathy syndrome (PRES), seizures, visual disturbance, cortical blindness, aphasia or ataxia.
Particularly in hemoglobinopathies (thalassemia, SCD) the reported incidence is around 30%, possibly also due to impaired hepatic metabolization of CsA and FK506 based on iron overload. However, also infusion modalities might impact on NT, since it was more frequently reported after 4-hours bolus injections (10.3%) than continuous infusion (3.3%). However, the excessive NT observed in SCD might be also related to the systemic vasculopathy, increasing with age and pro-inflammatory triggers after allo-HSCT.
Methods: A total of 30 pts aged 3 to 31 years with homozygous SCD or HbS 0/+ ß-Thal were treated between 2012 and 2018. Nine pts received a MSD bone marrow (BM) graft, 21 pts received T-haplo-HSCT from a relative (1 second T-haplo-HSCT due to graft rejection) with a α/β CD19 or CD3/CD19 depleted graft. Post-HSCT immunosuppression consisted of either CsA in 6 MSD and 16 T-haplo-HSCT pts or FK506 in 3 MSD and 6 T-haplo-HSCT pts, both mostly in combination with mycophenolate mofetil (MMF). FK506 was administered as a 20-hours continuous infusion, while CsA was given as 4-hours bolus injections. Dosage was adjusted according to usual target levels (CsA: 120ng/ml; FK506: 7ng/ml). Duration of immunosuppression was >6 months in T-haplo-SCT and <6 months in MSD, depending on chimerism. All pts developing neurological symptoms indicative for severe CNI-related NT underwent neuroradiological imaging (MRI/CT) with consecutive symptomatic treatment as indicated.
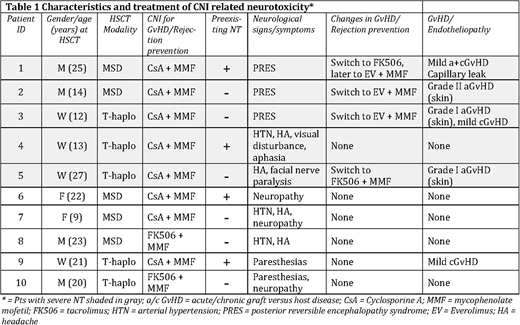
Results: Overall CNI-related NT was observed in 32.3% of our HSCT pts. Severe NT such as PRES and visual disturbance combined with aphasia was present in 16.1% (Table 1). Overall, NT was more prevalent in MSD (n=5, 55.5%) than in T-haplo-HSCT pts (n=5, 22.7%). The majority of NT events was observed under CsA prophylaxis (8/10; 80%) and in only 22% (2/9) pts with FK506. All 5 cases of severe NT, particularly all PRES, occurred on CsA. Complete recovery of neurologic symptoms was achieved in all pts spontaneously or after switching CsA to FK506 or everolimus (Table 1). Moreover, 60% of pts with NT was >18 years, and 90% >12 years suggesting an increasing risk with age while a third of patients with pre-existing NT experienced no post-HSCT NT. Of note, 4 of 5 pts with severe NT also experienced a mild acute GvHD (Table 1). The overall (OS) and disease-free survival (DFS) with a median follow-up of 17 months in T-haplo-HSCT pts and 22 months in 9 MSD HSCT pts was 90% vs. 100%, respectively.
Conclusions: Our data confirm an elevated risk for NT in SCD pts following allo-HSCT. Importantly, the incidence of NT events seems to be related to age (90% of pts with NT were >12years), donor source (MSD vs. T-Haplo; 55.5% vs 22.7%) and CsA rather than FK506 (CSA 80% vs. FK506 20%). All severe NT (particularly all PRES) were observed in pts with CsA prophylaxis, while the continuous infusion of FK506 might have levelled concentration peaks. Nevertheless, the NT observed with CsA post-HSCT could be the consequence of predominantly CsA-related vascular complications inflicting systemically pre-damaged vessels of SCD pts. The mechanism of action could be similar to other systemic endotheliopathies such as sinusoidal obstruction syndrome (VOD/SOS), transplant-associated microangiopathy (TAM) and acute GvHD which was observed in 4/5 pts with severe NT, compared to an overall GvHD rate of 29%.
Corbacioglu:Gentium: Consultancy, Honoraria; Jazz Pharmaceuticals: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal